James Barber is a therapeutic radiographer working in London in the UK. He’s a cisgender gay man who is passionate about representation and equality. James shared with us the work he’s been involved in to make informed consent forms for radiation therapy more inclusive for LGBTQ+ patients undergoing cancer treatment.
James reviewed the existing consent forms for various cancer sites and found they didn’t provide the same level of clinical consideration to patients in the LGBTQI+ community as to heterosexual and cisgender patients. One area which required review was the use of gendered language for treatment sites associated with the male or female gender, such as prostate, breast and gynaecological cancers. James says “As a gay cis-man there are aspects of this which I felt well placed to review and offer suggestions on.” We talked to James about the process and the inclusive language changes…
When you reviewed the existing radiotherapy consent forms, what stood out to you as being particularly cisnormative and heteronormative?
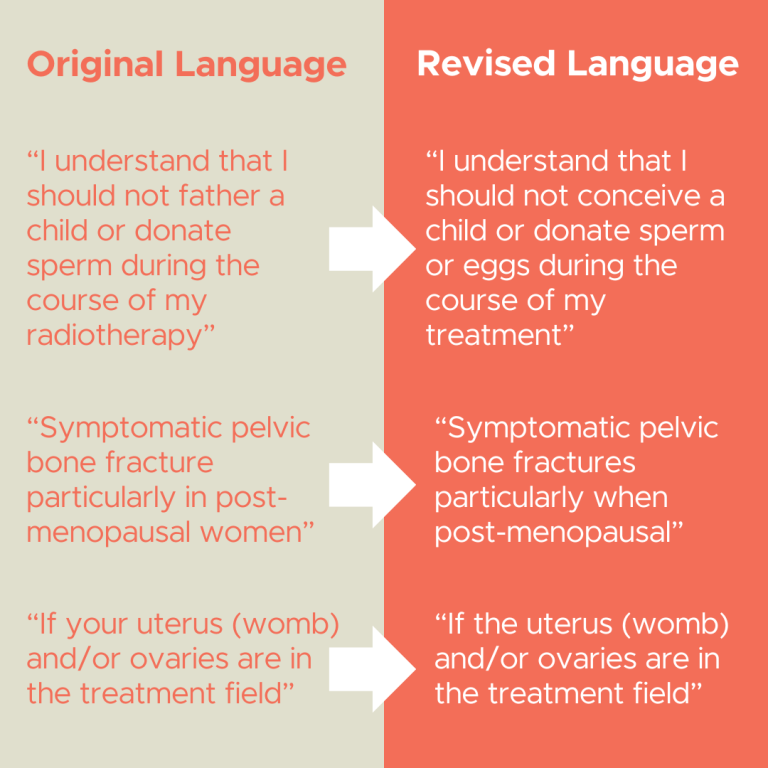
JB: One of the main things that initially stood out to me was the heteronormative nature of the sexual activity sections. Particularly in the gynaecological consent forms there was reasonably detailed discussion on the impacts of vaginal sexual function during and after radiotherapy, however when looking at the pelvic consent forms, particularly those for radiotherapy to the prostate, rectum and anal canal, there was not equivalent consideration given to the impact on receptive anal sex. When I then started looking in more detail through an LGBTQI+ inclusive lens, there were various other areas which used hetero and cis-normative language, such as the term “fathering a child” which was used on all consent forms except gynaecological and breast and the use of female gendered terms when discussing internal reproductive organs when referring to internal reproductive organs.
When suggesting changes to the consent forms, did you encounter any resistance?
JB: Generally the team were very good and receptive to suggested changes. I wouldn’t necessarily call it resistance, but the only push-back I had was around changing the way that gendered sexual organs were referred to – so moving away from “your” to “the”. Once we had had a discussion around the rationale for this and I had explained that this was to assist with minimising the psychological impact of this diagnosis on trans patients who may have pre-existing gender dysphoria relating to organs associated with their sex at birth which would then often be magnified by a cancer diagnosis linked to their sex at birth, they were very happy to take this forwards.

How long was the process from start to finish? What were the most time consuming aspects?
JB: The whole process probably took a few months, but that was mostly waiting for the relevant groups to meet up and review things. The most time consuming part of the process for me was reading through all of the consent forms in detail in a way that I had not done before, along with some of the initial EDI feedback notes from other experts in this area from when the forms were first developed, and trying to come up with constructive solutions to address the ways that they could be improved without leading to making the consent forms impracticably long, as firstly I knew that this would reduce the likelihood of the changes being accepted and secondly from first hand experience of clinical practice I knew that this was not desirable.
What advice would you give to someone wanting to revise consent form language to make them more inclusive?
I think the most important thing you can do is to try and think about all of the different groups that the consent form could apply to and then read it through once for each group with them in mind, looking in detail at how they would interpret and feel about things that as healthcare professionals we can very easily skim past. Even better if you can seek advice from people with relevant lived experience.
Find out more!
View and download the UK’s national radiotherapy consent form templates here: The Royal College of Radiologists News Article
Some more background on the project can be found here: The Society and College of Radiographers
James discusses the project on this podcast episode of RadChat with Jo McNamara and Naman Julka-Anderson

James leads ‘Equalise’ the Equality and Diversity Network of the Society of Radiographers (SoR). Here he is pictured at London’s Pride Parade representing the SoR with other group members.
HAPPY PRIDE!


